Vascular dementia
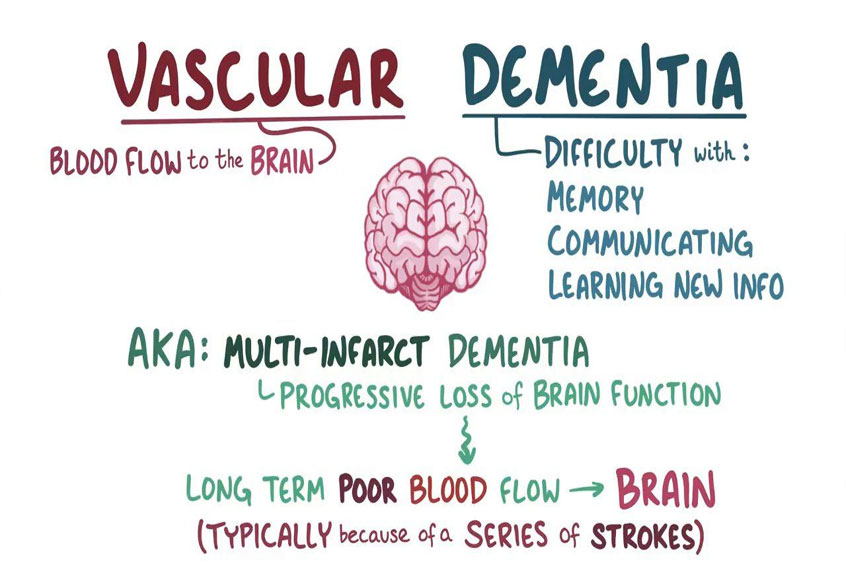
Vascular dementia is one of the most common forms of dementia, ranking only second to Alzheimer’s disease. Vascular dementia is caused by chronic, reduced blood flow to the brain-usually as the result of a stroke or series of strokes. In many cases, the strokes are so small that you may not notice any symptoms. These are known as “silent strokes.” But over time, the damage adds up, leading to memory loss, confusion, and other signs of dementia.
Vascular dementia represents a challenge for those affected by it and their caretakers. But with an understanding of the condition, and a willingness to make important lifestyle changes, it may be possible to prevent further blockages and compensate for brain damage that has already occurred.
What is vascular dementia?
Vascular dementia refers to a subtle, progressive decline in memory and cognitive functioning. It occurs when the blood supply carrying oxygen and nutrients to the brain is interrupted by a blocked or diseased vascular system. If blood supply is blocked for longer than a few seconds, brain cells can die, causing damage to the cortex of the brain-the area associated with learning, memory, and language.
Depending on the person, and the severity of the stroke or strokes, vascular dementia may come on gradually or suddenly. Currently, there is no known cure, but the good news is that making certain lifestyle changes and using practical strategies may help prevent strokes, compensate for cognitive loses, and slow its development.
Factors that increase your risk of heart disease and stroke – including high blood pressure, high cholesterol and smoking – also raise your vascular dementia risk. Controlling these factors can help lower your chances of developing vascular dementia.
The most common type of vascular dementia is multi-infarct dementia (MID), which is caused by a series of small strokes, or “mini-strokes,” that often go unnoticed and cause. These mini-strokes, also referred to as transient ischemic attacks (TIAs), result in only temporary, partial blockages of blood supply and brief impairments in consciousness or sight. Over time, however, as more areas of the brain become damaged, the symptoms of vascular dementia begin to appear.
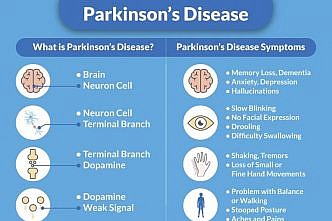
Signs and symptoms of vascular dementia
Vascular dementia affects different people in different ways and the speed of the progression varies from person to person. Some symptoms may be similar to those of other types of dementia and usually reflect increasing difficulty to perform everyday activities like eating, dressing, or shopping.
Behavioral and physical symptoms can come on dramatically or very gradually, although it appears that a prolonged period of TIAs-the mini-strokes discussed above-leads to a gradual decline in memory, whereas a bigger stroke can produce profound symptoms immediately. Regardless of the rate of appearance, vascular dementia typically progresses in a stepwise fashion, where lapses in memory and reasoning abilities are followed by periods of stability, only to give way to further decline.
Vascular dementia symptoms vary, depending on the part of your brain where blood flow is impaired. Symptoms often overlap with those of other types of dementia, especially Alzheimer’s disease. Vascular dementia symptoms may be most clear-cut when they occur suddenly following a stroke. When changes in your thinking and reasoning seem clearly linked to a stroke, this condition is sometimes called “post-stroke dementia.”
Another characteristic pattern of vascular dementia symptoms sometimes follows a series of strokes or mini strokes. In this pattern, changes in your thought processes occur in noticeable “steps” downward from your previous level of function, unlike the gradual, steady decline that typically occurs in Alzheimer’s disease.
But vascular dementia can also develop very gradually, just like Alzheimer’s disease. What’s more, vascular dementia and Alzheimer’s often occur together. Studies show that people with dementia symptoms usually have brain changes typical of more than one type. Some doctors call this condition “mixed dementia.”
Common mental and emotional signs and symptoms of vascular dementia
- Slowed thinking
- Memory problems; general forgetfulness
- Unusual mood changes (e.g. depression, irritability)
- Trouble paying attention and concentrating
- Decline in ability to analyze a situation, develop an effective plan, and communicate plan to others
- Hallucinations and delusions
- Confusion, which may get worse at night.
- Personality changes and loss of social skills
- Reduced ability to organize thoughts or actions
Common physical signs and symptoms of vascular dementia
- Dizziness
- Leg or arm weakness
- Tremors
- Wandering at night
- Moving with rapid, shuffling steps
- Balance problems
- Loss of bladder or bowel control
Common behavioral signs and symptoms of vascular dementia
- Slurred speech
- Language problems, such as difficulty finding the right words for things
- Getting lost in familiar surroundings
- Laughing or crying inappropriately
- Difficulty planning, organizing, or following instructions
- Difficulty doing things that used to come easily (e.g. paying bills or playing a favorite card game)
- Reduced ability to function in daily life
Causes of vascular dementia
Stroke, small vessel disease, or a mixture of the two can cause vascular dementia. Most commonly there is a blockage of small blood vessels somewhere in the vast system of arteries that feeds the brain and enters through the base of the skull. Blockages may be caused by plaque build up on the inside of the artery wall, or by blood clots which have broken loose and clogged a tributary further downstream. Clots can form as a result of abnormal heart rhythms, or other heart abnormalities. Also, a weak patch on an artery wall can balloon outward and form an aneurysm, which can burst and deprive the brain cells of oxygen.
It is estimated that about 50 percent of the cases of vascular dementia result from hypertension, or high blood pressure. Less common causes of vascular dementia are associated with autoimmune inflammatory diseases of the arteries such as lupus and temporal arteritis, which are treatable with drugs that suppress the immune system.
- Numbness, paralysis, or weakness on one side of your body or face.
- Trouble speaking (e.g. slurring your words, inability to repeat a simple sentence).
- Loss of vision or seeing double.
- Loss of balance and coordination (e.g. dizziness, trouble walking).
- Sudden, severe headache (may include a stiff neck, vomiting, or pain between your eyes).
Common conditions that may lead to vascular dementia include:
* Stroke (infarction) blocking a brain artery. Strokes that block a brain artery usually cause a range of symptoms that may include vascular dementia. But some strokes don’t cause any noticeable symptoms. These “silent brain infarctions” still increase dementia risk. With both silent and apparent strokes, the risk of vascular dementia increases with the number of infarctions that occur over time. One type of vascular dementia involving many strokes is called multi-infarct dementia.
* Narrowed or chronically damaged brain blood vessels. Conditions that narrow or inflict long-term damage on your brain blood vessels can also lead to vascular dementia. These conditions include the wear and tear associated with aging; high blood pressure; hardening of the arteries; diabetes; lupus erythematosus; brain hemorrhage; and temporal arteritis.
Risk factors
Certain factors can increase a person’s risk of developing dementia. These include:
- a medical history of stroke, high blood pressure, high cholesterol, diabetes (particularly type II), heart problems, or sleep apnea (where breathing stops during sleep)
- a lack of physical activity, drinking more than recommended levels of alcohol, smoking, eating a fatty diet, or leaving conditions such as high blood pressure or diabetes untreated
- a family history of stroke or vascular dementia
- an Indian, Bangladeshi, Pakistani, Sri Lankan or African-Caribbean ethnic background.
In general, the risk factors for vascular dementia are the same as those for heart disease and stroke.
Risk factors for vascular dementia include:
- Increasing age. Your risk for vascular dementia rises as you grow older. The disorder is rare before age 65, and risk rises substantially as you reach your 80s and 90s.
- History of heart attack, strokes or mini strokes. If you’ve had a heart attack, you may be at increased risk of having blood vessel problems in your brain. The brain damage that occurs with a stroke or a mini stroke (transient ischemic attack) may increase your risk of developing dementia.
- Atherosclerosis. This condition occurs when deposits of cholesterol and other substances (plaques) build up in your arteries and narrow your blood vessels. Atherosclerosis can increase your risk of vascular dementia – and possibly your risk of Alzheimer’s disease – by reducing the flow of blood that nourishes your brain.
- High cholesterol. Elevated levels of low-density lipoprotein (LDL), the so-called “bad” cholesterol, are associated with an increased risk of vascular dementia, and possibly with a higher risk of Alzheimer’s disease.
- High blood pressure. When your blood pressure’s too high, it puts extra stress on blood vessels everywhere in your body, including your brain. This increases the risk of vascular problems in the brain.
- Diabetes. High glucose levels damage blood vessels throughout your body. Damage in brain blood vessels can increase your risk of stroke and vascular dementia.
- Smoking. Smoking directly damages your blood vessels, increasing your risk of atherosclerosis and other circulatory diseases, including vascular dementia.
- Atrial fibrillation. In this abnormal heart rhythm, the upper chambers of your heart begin to beat rapidly and irregularly, out of coordination with your heart’s lower chambers. Atrial fibrillation increases your risk of stroke by leading to poor blood flow to your brain and elsewhere in your body.
Different types of vascular dementia
There are two main types of vascular dementia: one caused by stroke and one caused by small vessel disease. A third type is a mixture of the two. There are many other types of vascular dementia.
Stroke-related dementia
Stroke is the term used to describe permanent brain damage caused by an interruption in the supply of blood to specific parts of the brain. The symptoms that a person experiences as a result of a stroke depend on which area of the brain has been damaged. If the area in question is responsible for movement of a limb, paralysis might occur. If it is responsible for speech, the person might have problems communicating. Equally, damage to particular areas in the brain can cause the symptoms of dementia.
When vascular dementia is caused by a single stroke, it is sometimes called single-infarct dementia. Vascular dementia can also be caused by a series of small strokes. These can be so tiny that the person might not notice any symptoms, or the symptoms may be only temporary. This is called multi-infarct dementia.
Always consult a doctor if you experience any sudden symptoms, such as slurred speech, weakness on one side of the body, or blurred vision – even if they are only temporary. These episodes may be caused by temporary interruptions in the blood supply within the brain, known as transient ischaemic attacks. If left untreated, they can lead to permanent damage.
Small vessel disease-related dementia
This type of dementia, also known as sub-cortical vascular dementia or, in a severe form, Binswanger’s disease, is caused by damage to tiny blood vessels that lie deep in the brain. The symptoms develop more gradually and are often accompanied by walking problems.
Vascular dementia and Alzheimer’s disease (mixed dementia)
A diagnosis of mixed dementia means that Alzheimer’s disease, as well as stroke or small vessel disease, may have caused damage to the brain.
Treatment
Controlling underlying conditions and risk factors
Controlling conditions that affect the underlying health of your heart and blood vessels can sometimes slow the rate at which vascular dementia gets worse, and may also sometimes prevent further decline. Depending on your individual situation, your doctor may prescribe medications to:
- Lower your blood pressure
- Reduce your cholesterol level
- Prevent your blood from clotting and keep your arteries clear
- Help control your blood sugar if you have diabetes
Alzheimer’s medications
The Food and Drug Administration (FDA) has not approved any drugs specifically to treat changes in judgment, planning, memory and other thought processes caused by vascular dementia. However, certain medications approved by the FDA to treat these symptoms in Alzheimer’s disease may also help people with vascular dementia to the same modest extent they help those with Alzheimer’s.
Doctors may prescribe one or both types of the following Alzheimer’s drugs:
- Cholinesterase inhibitors – including donepezil (Aricept), galantamine (Razadyne) and rivastigmine (Exelon) – work by boosting levels of a brain cell chemical messenger involved in memory and judgment. Side effects can include nausea, vomiting, muscle cramps and diarrhea.
- Memantine (Namenda) regulates another brain cell chemical messenger important for information processing, storage and retrieval. Side effects can include headache, constipation, confusion and dizziness.
Prevention
The health of your brain’s blood vessels is closely linked to your overall heart health. Taking these steps to keep your heart healthy may also help reduce your risk of vascular dementia:
- Maintain a healthy blood pressure. Keeping your blood pressure in the normal range may help prevent both vascular dementia and Alzheimer’s disease.
- Keep your cholesterol in check. A healthy, low-fat diet and cholesterol-lowering medications if you need them may reduce your risk of vascular dementia, probably by reducing the amount of plaque deposits building up inside your brain’s arteries.
- Prevent or control diabetes. Avoiding the onset of diabetes, with diet and exercise, is another possible way to decrease your risk of dementia. If you already have diabetes, controlling your glucose levels can help protect your brain blood vessels from damage.
- Quit smoking. Smoking tobacco damages blood vessels everywhere in your body.
- Get physical exercise. Regular physical activity should be a key part of everyone’s wellness plan. In addition to all of its other benefits, exercise may help you avoid vascular dementia.